
About 5% of women are born with uterine structural abnormalities. This can impact their reproductive health and affect their ability to conceive and carry a pregnancy. So it is important to understand it and its potential implications. Continue reading to learn about uterine malformations, their types, causes, symptoms and more.

The uterus is different in each woman, but typically an adult woman has a uterus that is approximately 6-8 cm long and 5 cm wide. It resembles an inverted triangle. The endometrium thickness in women of reproductive age varies throughout the menstrual cycle, typically ranging from 4 to 16 mm depending on the phase. Also taken into consideration is whether a woman has had previous pregnancies, as that can cause irreversible cavity distension. For instance, a woman with multiple pregnancies, the uterus will be about 10 cm long and 7 cm wide.
Uterine malformations, also called Mullerian malformations, are a congenital anomaly as the uterus does not form properly before birth. It occurs due to problems in the development stages of the fetus, where the uterine structures do not form as they should. The Mullerian ducts are embryonic structures that are paired tubes that develop into the FRT (female reproductive tract) including the upper vagina, fallopian tube, uterus and the cervix. These ducts fuse to make a central uterine cavity during fetal development. The disruption of this process leads to many kinds of uterine malformations.
These are called Mullerian anomalies and cause issues with reproductive system like vaginal septum or unusual structures. These are malformations formed before birth and affect the way the uterus functions, leading to various malformations in the reproductive organs.
In most cases, the cause of congenital uterine malformations is unknown. Women with these anomalies have normal chromosome quantity. During 1938-71, DES (diethylstilbestrol) was used to prevent miscarriages and preterm deliveries in some women. Women exposed to DES in the womb are at a greater risk of uterine anomaly. There are no major risk factors for this condition.
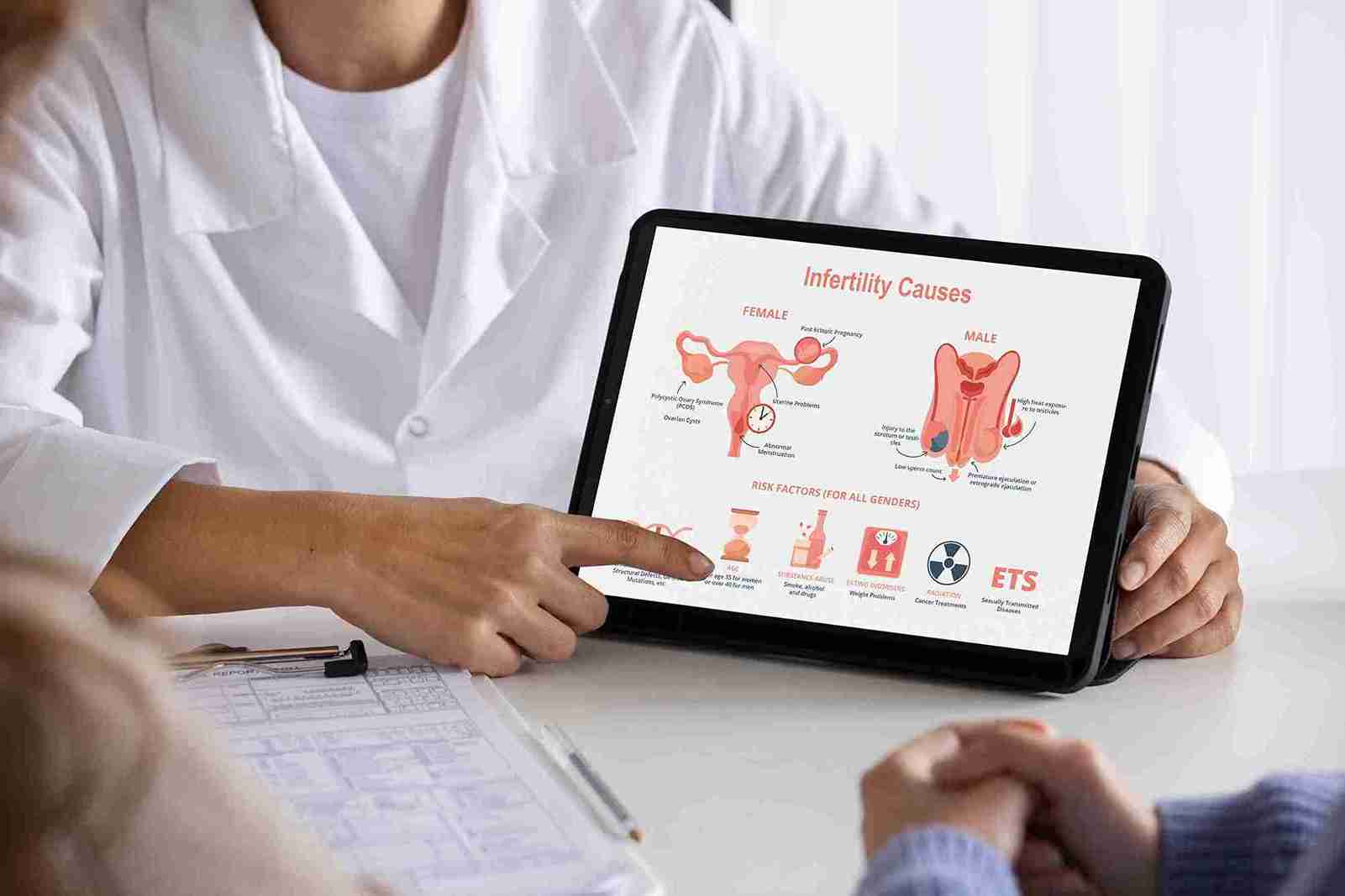
Most cases of uterine anomalies are not serious, do not lead to fertility issues, and hence go unnoticed. Additionally, in some cases, due to mild malformations, there are no associated symptoms. However, it is also true that they are not a rare or isolated problem. Studies suggest that uterine abnormalities may contribute to approximately 10-15% of fertility challenges. This condition is often identified only when a woman experiences fertility challenges. Even if she gets pregnant, uterine malformations can lead to:
● Ectopic pregnancies
● Implantation failures
● Abortions
● Premature birth
● Fetal malpositions
● Dysdynamics and other such complications
Due to the above problems, fertility specialists perform tests to give a proper diagnosis.

As the name indicates, the uterus is absent. This condition is called Müllerian agenesis or Mayer-Rokitansky-Küster-Hauser syndrome. Women with this anomaly will typically have functioning ovaries and external genitalia, but do not have menstrual cycles and cannot carry a baby. In some women, the uterus is present but is not developed to its normal size or does not function, and is called uterine hypoplasia.
In this condition, externally the uterus looks normal, but internally it has a septum where the uterine cavity is divided into smaller cavities, unlike a normal uterus. During fetal development, the Mullerian ducts are fused, but a partition is present that causes the uterus to split into two. Women with uterine septum have the worst outcome, with low fetal survival and higher premature birth. It is also the most common cause of miscarriages.
Women with an arcuate uterus have a normal-looking uterus externally but have a slight fundal indentation of 1cm or less. Most research indicates this variation rarely impacts fertility, though in some cases, there may be a slightly higher risk of miscarriage. It is one of the least severe types of uterine anomalies and does not cause any major reproductive issues.
It is a common Mullerian malformation type characterised by a womb with two horns. Instead of pear-shaped, the uterus is heart-shaped, with a deep indentation. This shape does not allow enough space for the baby to grow compared to a normal shape.
This condition happens when one of the Müllerian ducts does not form or develops partially. This results in a uterus that is smaller than normal, shaped like a banana, with a single fallopian tube.
Also called double uterus or uterus didelphys, the Mullerian ducts do not fuse despite developing. This means women end up having double uterus with each having a cervix and seperate vaginas.
Uterine malformations typically present no symptoms. Some women easily get pregnant and discover that they have an unusually shaped uterus during a prenatal ultrasound. Others get a diagnosis when they go for fertility issues. Other uterine anomalies symptoms include:
● Fertility issues
● Recurrent miscarriages
● Amenorrhea
Uterine malformations are recognised during puberty when a young woman fails to have her first period or does not have regular menstrual periods. It can also be diagnosed later due to difficulty in conception or maintaining pregnancy. Some malformations are linked with pelvic pain, menstrual abnormalities, and discomfort during intercourse. To get an accurate diagnosis, a combination of medical tests is recommended. Some of them are:
MRI: Most recommended test as it allows evaluation of the external contour, pelvic anatomy, and junctional zone.
Ultrasound: Provides clear images of the uterus, helping the doctor accurately identify the uterine malformation type. Less invasive, this is preferred over MRI if high-quality imaging is needed.
Hysteroscopy: Useful in diagnosing malformations like polyps or septums, and helps treat certain conditions immediately.
Surgical intervention, when indicated, is the primary treatment for uterine malformations. However, not all cases require surgery. Uterine anomalies may lead to fertility issues; however, many women with this condition have successful pregnancies with/without surgery.
● Surgery is not recommended for a didelphic uterus.
● A uterine septum can be corrected using a combination of hysteroscopy and laparoscopy. This procedure reduces Mallerian duct malformations and reduces the miscarriage rates.
● Surgery is recommended for a septate uterus as it can be corrected with improved chances of pregnancy outcomes.
● Women who have a congenital reproductive malformation and are unable to get pregnant can opt for surgery. It can repair anomalies, reduce discomfort during periods, and enhance fertility and pregnancy success.
● Surgery is not recommended for those with didelphic malformations or unicornuate, bicornuate malformations.

Uterine malformations may or may not lead to fertility issues and pregnancy complications. If it causes fertility issues, it can be accurately diagnosed with the help of newer imaging tests. These tests help to diagnose and treat complications caused by and ensure a healthy pregnancy.

These are congenital uterine abnormalities of the female reproductive tract due to abnormal Mullerian duct development during fetal development.

Uterine malformations are caused by abnormal development of the Müllerian duct during the fetal developmental stage.

Absent uterus, Uterine Septum, Arcuate Uterus, Bicornuate Uterus, Unicornuate Uterus, and Didelphys Uterus are some types of uterine abnormalities.

About 5% of women are born with uterine structural abnormalities.